Written by Mae Lee (she/her/hers)
In honor of National Public Health Week 2022
In the 2003 film Freaky Friday, Lindsay Lohan switches body with her mom after eating a magic fortune cookie the night before, then attributes the switch to “strange Asian voodoo”. As a kid I thought, “Cool! People think I can do magic!”. It wasn’t until I grew older that I realized how harmful this mystification of cultures can be. This assumption that minorities have other worldly powers just solidifies that we are, in fact, not human. (And no, contrary to what 8-year-old me thought, it is not a compliment).
And while we can chalk Freaky Friday up to good ol’ racism intertwined with lazy scriptwriting, this superhumanization of minorities is especially harmful to Black Americans when receiving healthcare.
Myths such as “Black people have thicker skin than white people”, “Black people have less sensitive nerve endings”, and “Black people’s blood coagulates faster than white people” are rooted in 19th century experiments in which slaves were tortured under the guise of scientific discovery. This is a part of a line of experiments that sought to prove biological inferiority of Black people in order to push racist agendas. This is just one example of the weaponization of scientific rhetoric to support ulterior motives.
And you might say, “Hey! That was so long ago! Times are different now!” First off, don’t interrupt me, it’s rude. Second, I’d like you to take a moment and think back to the year 2016. Adele’s absolute banger “Hello” had just come out, Obama ended his second presidency, and a study in the Proceedings of the National Academies of Science found that over one third of the surveyed 1st and 2nd year medical students endorsed the belief one or more of the myths mentioned above. These are the doctors that are practicing medicine in hospitals today.
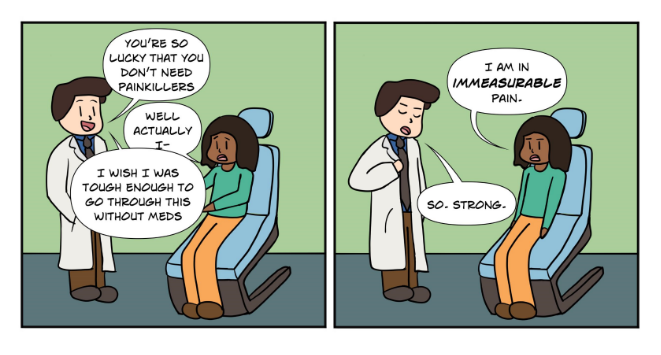
This widespread bias leads to Black people commonly being under prescribed pain medication. In fact, in the aforementioned study, the medical students who endorsed these beliefs rated Black people’s pain less than that of White people in the same situation, resulting in less accurate treatment recommendations. Believing that Black people have some superhuman ability to shield pain causes doctors to underestimate their pain, and thus causes them to under prescribe pain medication to their Black patients.
Data from the National Hospital Ambulatory Medical Care Survey over a 5-year period showed that Black people were half as likely to be prescribed opioids for back and stomach pain when compared to White people. This failure to prescribe the same amount of medication in the same situation across races starts at a very young age. JAMA Pediatrics conducted a study which showed that Black and Latinx kids were less likely to receive pain medication than white children.
Even if you know your doctor is under-prescribing you pain medication, trying to convince your doctor of your pain is a whole other issue. This would be especially difficult for patients who suffer anxiety or cannot confront authority. Imagine trying to tell a doctor that their diagnosis is incorrect, when the entire medical system reinforces myths about your body that you know aren’t true. The hospital or the emergency department is the doctor’s space. They have the power, the medical knowledge, their diploma on the wall. Think about trying to push back against this power imbalance by explaining a sensation that nobody else has access to. Now do it while being in excruciating pain.
An accompanying problem is the prevalent stereotype that associates Black people with urban crime and drug addiction. This can cause doctors to be more hesitant when prescribing narcotics to Black patients. Rather than seeing a patient in pain, they see a drug addict faking it for their next fix, despite pushback from their patients. This implicit bias is exacerbated by the lack of diversity in the medical field. There is an overwhelming lack of Black doctors and dentists in the field. The racial makeup of medical professionals does not reflect the populations they serve. This is especially harmful because of in-group bias – bias in favor of people who look like you. In a study performed in 2019, white participants were able to recognize pain more accurately in photos of White patients compared to photos of Black patients. If the racial makeup of medical professionals continues to consist predominantly of White people, Black patients will continue to be misdiagnosed and mistreated.
There is also this concept of the “strong, independent, Black woman”. And while this image can be empowering, it also serves to undermine the pain that Black women go through, either physically or mentally. Over-idolizing groups can harm them. Humans struggle. Humans feel pain. Assuming Black people aren’t subject to these things denies them of their experience and of receiving the appropriate help. It robs Black people of their humanity and otherizes them. Black pain needs to be taken more seriously, and pain medication is just one of the avenues in which racism lives in public health.
Hmm, makes me wonder why Luke Cage, one of Marvel’s few black superheroes, has a superpower that enables him to not feel pain.