Written by Tonayo Crow
As the COVID-19 vaccine rollout gains momentum in the United States and a pandemic-free future emerges from the haze of this past year, we are facing the reality of a nation that needs to rethink its public health system if we want to respond more effectively to future diseases and health threats. Taking a step back, it is important to acknowledge that not every country has the luxury yet to look to the future—high-income nations have purchased over half of the global vaccine supply despite having only 19% of the world’s adult population, and experts estimate that some people (especially those in lower-middle income nations) may be waiting until 2023 for a vaccine. This is just one of many examples of the glaring inequities that were exposed by the pandemic. So how do we rethink the role of public health in people’s lives, when the U.S. dedicates less than 3% of health spending to public health?
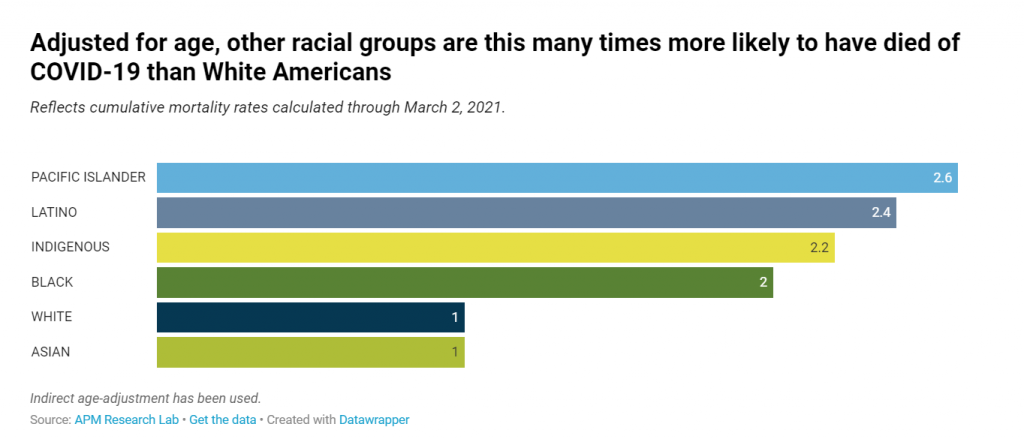
The first step is to invest in public health and recognize the value of preventative efforts, which aim to address the Social Determinants of Health upfront instead of waiting until there’s a problem that needs fixing (e.g. intentionally building communities with heavy tree cover to combat the effects of extreme heat). However, we cannot forgo equity in this process; we must center it. Despite the initial belief that COVID-19 would hit everyone equally (after all, a virus just wants a willing host), we now know that that is not how the pandemic played out—Black, Pacific Islander, Latinx, and Indigenous populations have and are suffering disproportionate COVID-19 death and infection rates compared to white populations. If we want to reimagine public health in the United States, we need to invest in a public health system that prioritizes prevention, uplifts community voice, and centers racial equity.
American h ealthcare often focuses on treating symptoms, not root causes. For example, a child taken to the doctor for asthma may be proscribed medicine and advised not to engage too heavily in any activities that will exacerbate their symptoms, but how often does the doctor push further and ask—where is the child playing, learning, and living? We know that race is the number one indicator for the placement of toxic facilities in the U.S., and that the pollutants emitted from those plants can cause or worsen asthmatic symptoms and other respiratory illnesses. So it should come as no surprise that Black, Latinx, and Indigenous children experience higher rates of asthma than their white counterparts. This is where public health comes in.
ealthcare often focuses on treating symptoms, not root causes. For example, a child taken to the doctor for asthma may be proscribed medicine and advised not to engage too heavily in any activities that will exacerbate their symptoms, but how often does the doctor push further and ask—where is the child playing, learning, and living? We know that race is the number one indicator for the placement of toxic facilities in the U.S., and that the pollutants emitted from those plants can cause or worsen asthmatic symptoms and other respiratory illnesses. So it should come as no surprise that Black, Latinx, and Indigenous children experience higher rates of asthma than their white counterparts. This is where public health comes in.
Increasing public health spending helps create a healthier nation by supporting population-level health (by addressing systems-level issues instead of bandaging problems) and also makes good economic sense. If COVID-19 taught us anything, it’s that a more organized, well-funded, and cohesive public health effort could have prevented numerous deaths. We know that public health preventions work: mask-wearing and social distancing saves lives. Removing leaded pipes from communities prevents disease and death from lead poisoning. Building communities with walkable sidewalks and green space encourages physical activity and boosts mental health. Removing polluting plants from places where people live creates cleaner air for children to breathe. In order to protect the health of all people, we need a more robust public health system.
 But what does this look like? Firstly, we should look to community leaders that are already fighting for better health for themselves and their neighbors. Local, state, and federal public health workers need to work collaboratively with communities, instead of making assumptions about what communities need. Further, as mentioned above, racial equity must be central to public health work. Racism is a public health crisis, and race is a determining factor for health outcomes. This means that, due to historic, systemic inequities, your race can be an indicator for a negative health outcome, regardless of your individual behavior. Racial inequity exists across all systems (health, education, workforce, etc.) and socio-economic status does not account for this inequity (to illustrate with a stark example, Black women, regardless of income, are three times as likely as white women to die from pregnancy and childbirth complications). If we don’t continue using public health work as an avenue to fight systemic racism, then there is little hope to combat the centuries of systemic barriers to good health for BIPOC (Black, Indigenous, and People of Color) folks in the United States.
But what does this look like? Firstly, we should look to community leaders that are already fighting for better health for themselves and their neighbors. Local, state, and federal public health workers need to work collaboratively with communities, instead of making assumptions about what communities need. Further, as mentioned above, racial equity must be central to public health work. Racism is a public health crisis, and race is a determining factor for health outcomes. This means that, due to historic, systemic inequities, your race can be an indicator for a negative health outcome, regardless of your individual behavior. Racial inequity exists across all systems (health, education, workforce, etc.) and socio-economic status does not account for this inequity (to illustrate with a stark example, Black women, regardless of income, are three times as likely as white women to die from pregnancy and childbirth complications). If we don’t continue using public health work as an avenue to fight systemic racism, then there is little hope to combat the centuries of systemic barriers to good health for BIPOC (Black, Indigenous, and People of Color) folks in the United States.
Rebuilding after COVID-19 means taking a serious, introspective look at what, and who, is prioritized in this country, and investing more resources in communities of color that have historically been underserved or ignored entirely. Public health can be a force of good if we invest in it, and the health of individuals and communities across the United States depends on it. As we look to the future, we cannot ignore the lessons of this past year. So let’s start rebuilding, and create a better funded, more equitable public health system that works for everyone.